by Chris Durst Nov. 18, 2020
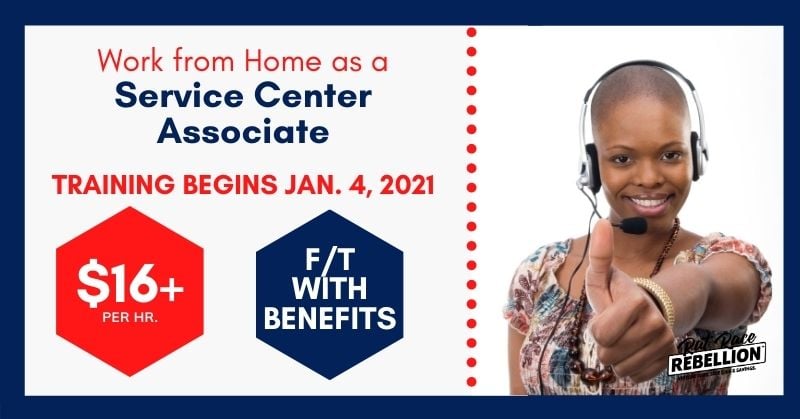
If you have a HS diploma or GED and you’d like to work from home for a larger company, Sedgwick — which specializes in processing insurance claims — is hiring Service Center Representative.
No college required. No state hiring restrictions mentioned. Benefits included and they start on DAY ONE. “The work is so easy, it’s literally data entry,” Yabina I. posted to our Facebook page.
“Start date January 4, 2021.”
Pay is $16.31 per hour.
Here’s what the company has to say about these openings:
“For a career path that is both challenging and rewarding, join Sedgwick’s talented team of 21,000 colleagues around the globe. Sedgwick is a leading provider of technology-enabled risk, benefits and integrated business solutions. Taking care of people is at the heart of everything we do. Millions of people and organizations count on Sedgwick each year to take care of their needs when they face a major life event or something unexpected happens. Whether they have a workplace injury, suffer property or financial loss or damage from a natural or manmade disaster, are involved in an auto or other type of accident, or need time away from work for the birth of a child or another medical situation, we are here to provide compassionate care and expert guidance. Our clients depend on our talented colleagues to take care of their most valuable assets — their employees, their customers and their property. At Sedgwick, caring counts®. Join our team of creative and caring people of all backgrounds, and help us make a difference in the lives of others.
PRIMARY PURPOSE: To provide excellent service to callers regarding claims for multiple lines of business; to expedite the claims application process and provide detailed claim notes on all calls; to resolve issues with one call/one person response; and to direct calls to appropriate escalation path as needed.
ESSENTIAL FUNCTIONS and RESPONSIBILITIES
- Acts as primary liaison with callers; follows client specifications in assisting with questions and solving problems related to the claims application and servicing processes.
- Educates and informs the customer multiple communication channels about documentation required to process a claim, required time frames, payment information, and claim status.
- Educates claimants/callers on client requirements and benefit plans documenting all required details of the call in a concise professional manner.
- Enters verbal and written application information that meets both the internal and external customer’s requirements accurately into the claims management system.
- Assigns new claims to the appropriate claims handler.
- Directs customer calls to the appropriate contact at multiple locations or escalates to Service Center
- Specialist/management as needed.
- Attendance during scheduled work hours is required.
ADDITIONAL FUNCTIONS and RESPONSIBILITIES
- Performs other duties as assigned.
- Supports the organization’s quality program(s).
QUALIFICATIONS
- High school diploma or GED required. College courses preferred
Experience
- One (1) year customer service experience or equivalent combination of education and experience required. Inbound call center experience preferred.
Skills & Knowledge
- Knowledge of medical terminology
- Understanding of claims management
- Excellent oral and written communication skills
- PC literate, including Microsoft Office products
- Strong organizational skills
- Good interpersonal skills
- Ability to multi task in fast paced environment
- Ability to support multiple clients across communication channels and utilize multiple systems simultaneously
- Ability to work in a team environment and/or independently
- Ability to meet or exceed Performance Competencies”
CLICK HERE for full details and to apply. For more jobs like these, check our Newest Jobs & Gigs page. To be the first to hear about jobs like these, like our Facebook page. May you be working from home soon!
PLEASE SHARE this post – turn your friends into Rat Race Rebels!


Recent Comments